|
Heelspurs.com's position on surgery for plantar fasciitis and heel spurs is that no one should ever have surgery for these conditions unless they have read and tried everything in Scott's book.
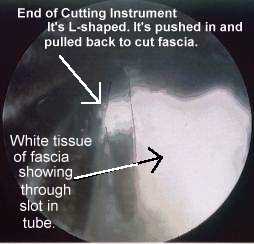
SurgeryMost surgeries will be replaced by ESWT because ESWT is safer and appears to have a higher success rate. 8% of our visitors have had surgery with a self-reported success rate of 37% to 60% depending on the type of surgery. About 20% have reported that surgery has made their condition worse. These results are much worse than what is reported in most journal articles, but closer to what some doctors are telling me through email. A serious problem with our visitor surveys in keeping track of the success rate of surgery is that it may take 6 months for the damage done by surgery to heal before improvement can be seen. It is likely that our visitors who currently say the surgery was a failure may later consider it a success but not come back to report it. Also, if surgery was a success, they would not be visiting the website and filling out a survey. But the same could be said for any of the other treatments which rank much better. If there is some truth to the survey results, an explanation for why our results are so much lower than what journals report could be that journal articles are about cases with specific symptoms. If our visitors do not typically have the same set of symptoms, then the surgery being studied in any particular article would be less comparable to our results. Out of necessity, doctors may be applying the various surgeries to a wider range of cases than was intended by the journal articles. Those publishing the studies are often those that have the most experience and skill in that type of surgery. Other doctors may not implement the surgery in the same way. A 3rd possibility is that patients and doctors have different opinions as to what constitutes a successful surgery. A 4th possibility is that patients overestimate the success of a surgery when speaking to their surgeon. In journal articles surgery is reported to have a success rate of 50% 17 to 97% 22, et al, depending on which source is quoted, which surgery is used, and on which doctor performs it. Endoscopic plantar fasciotomy (EPF) is the newest method. Other surgical techniques are still more common and require a larger incision (up to 2 inches) that takes longer to heal (after reading the message boards I get the impression 6 weeks to a year is required, or forever), but some doctors may prefer the older methods to endoscopic plantar fasciotomy because it allows them to see better and cut more accurately (and possibly to relieve nerve entrapment or remove the spur). There is also a "minimal incision" type of surgery that may be as beneficial as EPF and not as dangerous as other surgeries that require larger incisions. Several sources say surgery is ultimately required in about 10% of the cases, but many doctors claim it is needed in less than 5% of their patients. Most doctors require conservative treatment (which means no surgery, and usually it means no shots) for about 12 months before considering it. Endoscopic plantar fasciotomy is relatively new and requires equipment and skill that some doctors do not have. Some surgeons do not think it is more effective than other types of surgery, but there is at least one journal article that indicates otherwise. Our visitors do not rank it as well as heel spur removal surgeries, but the results are not statistically significant. It was first performed around 1991. It appears from our surgery database and journal articles that podiatrists are using it much more often than orthopedic surgeons. It takes 20 minutes to an hour and does not require a stay in the hospital. The surgeon detaches (cuts) a portion of the plantar fascia from the heel (this is the origin of the "plantar fasciotomy" portion of the EPF name). A slotted tube is inserted through two small incisions (less than 1/2") in the skin on each side of the heel. Sometimes an incision is made only on the inside of the heel. A knife inserted down the tube pokes out of the slot, cutting the fascia. An endoscopic camera is inserted into the tube to allow the surgeon to see what he is cutting (this is the origin of the "endoscopic" portion of the EPF name). The cut fascia usually relieves pain and pressure in the area. New fascia tissue grows into the gap created by the cut. Practice on cadavers is necessary. The two-portal (two incisions) method was patented by Dr. Barrett in 1993. Dr. Barrett says "Most patients return to their regular shoes in 3-5 days. Most return to work after the first week, and return to their normal activities by the end of the third week. Everyone heals slightly differently. Other factors such as age, weight, and occupation can contribute to healing times." In a 1995 J Foot Ankle Surg report Dr. Barrett reported 1 month was the average time required to return to work. This report indicated open heel surgery was not as effective. Footlaw.com states cuboid pain, nerve entrapment, severe arch discomfort, and post-traumatic nerve syndrome are all potentially serious complications of EPF (and possibly other fascia release surgeries), although it also states many patients are helped by the procedure. An orthopedic surgeon informed me that he saw about 500 cases of plantar fasciitis (heel spurs) in two years. 50% of his patients get better with better shoes, rest, NSAIDs, frequent massage, ice, and stretching. He subjects the other 50% to shots. Out of ten patients, 5 get the shots. 3 of those 5 are cured with the first shot. The other 2 get the second shot. One of those is cured. The last one (out of the initial ten) gets EPF surgery. He reports only 1 or 2 surgery failures out of 50. After the surgery, patients are walking the same day without pain (this is rare compared to visitors who post to this site). In 4 weeks their activities are back to normal without pain. He no longer performs surgery on both feet at the same time. EPF and other surgeries that release the fascia usually cut only the portion of the fascia over the inside front of the heel bone where the bone sticks out a little to connect to the fascia (a.k.a. "medial calcaneal tubercle"). In the past, detaching the entire fascia was more common but there were more frequent complications. It is debatable if non-EPF fascia release surgeries are more or less effective than EPF. I believe EPF is more effective, unless a particular doctor has perfected a minimal incision method. I do not think detaching the entire fascia from the heel would be wise in the majority of cases because of the fascia's important role in connecting the heel to the ball of the foot and thereby creating the arch in the bone structure of the foot. Complications for fascia release surgeries: The arch may fall some or have other problems after fascia release type surgeries (including EPF). Using arch support after surgery is recommended by some to help prevent the complications that result from a lowering of the arch. One journal article says surgery in those with flat feet may not be good (the exact quote is: "The data suggest that operations involving fasciotomy affect arch stability and should not be performed in patients with evidence of concomitant pes planus deformity, because of the likelihood of further deformation"). Wheeless' Orthopedic website says plantar fascia release (not nerve entrapment surgery or heel spur removal) "would appear to be an illogical procedure in patients w/ pes planus (flat feet)." The arch may drop some or other foot problems may result in addition to not curing the original problem. For example, I've had several visitors tell me the outside (lateral) edge of their foot starting hurting after the surgery. If the pain is near the bottom and outside edge of the foot, it could be because more tension is in the lateral band of the fascia. If the pain is on the top and outside edge of the foot above or in the arch, it could be pressure being placed on the cuboid bone caused by the lowering of the arch. Paper number 184 at the 1996 Annual Meeting of the American Academy of Orthopaedic Surgeons indicated the lateral side of the arch of the foot dropped 2.6 mm when only the medial band of the fascia was cut and that this was a possible cause of lateral arch pain after surgery (a joint and ligament on the lateral edge are experiencing more stress). The medial side of the arch dropped 4 mm. Here's a recent journal article's conclusion about fascia release surgery: Although plantar fasciotomies continue to be used to relieve the heel pain associated with plantar fasciitis, there are no criteria as to the amount of fascia release required to relieve symptoms while maintaining the integrity of foot function. .... The study demonstrated that partially releasing the plantar fascia imparts forces to the remaining fascia that are not usually observed with the fascia intact. .... When the plantar fascia was released, the subtalar joint was unable to resupinate in late midstance and propulsion, and there seems to be a direct correlation between the amount of fascia transected and the subtalar joint’s inability to resupinate. .... More research is needed to determine more precisely the amount of plantar fascia that can be released before significant increases in forces in the remaining fascia are observed and before loss of the subtalar joint’s ability to resupinate during late stance and propulsion. From this initial study, it seems that less than 66% of the fascia should be released to maintain foot stability, which is in agreement with in vivo research on lateral column symptoms following plantar fascial release. - Erin D. Ward, DPM et al, Journal of the American Podiatric Medical Association, Vol 93 #6 429-442 2003 Heel spur removal surgery (a.k.a. "inferior calcaneal exostectomy") is often used, but some sources since 1990 indicate they should not be removed. According to doctor Lundeen (www.drlundeen.com) "Beware if a surgeon says the spur needs to be removed...." A journal article says "Radiographically [by x-ray] it was noted that, despite complete excision, subcalcaneal exostoses [heel spurs] often reformed ... findings of this study suggest that changes within the fascia, rather than the spur, are primarily responsible for the pathogenesis of the syndrome." And "not in any case the calcaneal [heel] spur found [by X-ray] induces pain or tenderness. ... Results of the surgical removal of the painful calcaneal heel spurs have been disappointing. ... Since chiselling down the calcaneal [heel] spur also removes the attachment of the plantar aponeurosis [fascia], patients must accept subsequent lowering of the arch of the foot." Another journal article abstract: "Four patients developed calcaneal fractures while walking, soon after bone removal from the under-surface of the calcaneus. Heel spur or osteomyelitic bone removal can lead to this complication." Should heel spurs be removed? I don't know. Our visitors rank heel spur removal higher than all the other surgeries. A visitor emailed to say his doctor performs 150 heel spur removals a year "without cutting the fascia" with apparently good success. I do not know anything about surgeries directed toward nerves to relieve pain due to nerve "entrapment" or "involvement" and cannot comment, except to say they ranked the worst among the surgeries reported by our visitors. In any surgery, a nerve may be cut during surgery or inflammation from surgery may put pressure on the nerve and cause pain, loss of sensation, and/or tingling in the bottom of the foot or in the toes. The doctor may call it "peripheral neuropathy". It is not necessarily permanent damage. Surgery may also injure arteries and veins that allow good blood supply and thereby increase healing time or cause deadening of tissue. This may be called "avascular necrosis". Immediately after sugery I would apply ice as much as possible for 2 days in order to keep the injury cool and to help it heal faster and stronger. I would also take it very easy (rest the feet) before slowly increasing activity in the absence of pain and listen carefully to the doctor's instructions. I would seriously consider arch support and tape. Vitamin C is important for scar tissue to heal back strong. It is required in several of the steps in collagen formation. 4,000 mg spread out over each day may help if taken for at least a fews days following surgery, but preferably for weeks. It used to be used in conjunction with all surgeries in the 50s. For more info see my vitamin C rant. The first two pictures below are what doctors see on a TV monitor when doing EPF.
heelspurs.com | 
|