This is part 2 of a 2-part document that can be printed out. Part 1.
Table of Contents
|
Decreasing activity (a.k.a. rest), ice, stretching the calf muscles without re-injuring the fascia, and/or better arch support are often the cure for plantar fasciitis (heel spur). The following list is approximately in the order of most effective treatments reported by our visitors' survey responses.
The following sections expand on some of the above.Decreasing ActivityFoot problems are often difficult to cure because the feet never get a rest. Most treatments are simply different ways of giving the fascia rest. Healing can easily require months of reduced activity. My best method of resting the fascia has been to use tape. Some sources strongly recommend never walking barefoot without arch support (and possibly a heel pad) to prevent re-injury. With too much rest, muscles, ligaments, tendons, and the fascia lose strength. Nevertheless, many visitors have reported a method similar to the following is a cure:
Stretching the Calf MusclesStretching the calf muscles is needed in most cases of plantar fasciitis (heel spur). Studies show between 70% and 90% of patients improve with stretching. Stretching is not needed if the foot can bend back more than 25 degrees (see further below for how to measure your flexibility). If there is pain with the first few steps in morning, massage and stretching the fascia itself before getting out of bed by bending the toes and foot back with a towel (with the ends held in the hands and looped around the feet) may help. If it does not increase the pain, stretches can be thirty seconds long, with 15-second breaks, repeated three times with the legs straight (knees not bent - a tight gastroc calf muscle instead of soleous is the one that causes heel pain). Some sources say to also do it with the knees bent (soleous), but I think they are in error because the knee appears in the straight, locked position when the flexibility issue is important (right before the heel comes off the ground). Stretching can be done three times a day or more if done gently. Several who have desk jobs have emailed to say that stretching before walking was crucial to their recovery. All sources recommend against bouncing while stretching. Stretching several times for only 30 seconds with 15 seconds breaks is a frequently recommended approach. I have much more success holding stretches for two minutes twice a day. Standing with the balls of the feet on an edge like a step and lowering the heels is probably the best and easiest method....and you can see your flexibilty increase after a minute of two. It may be best for everyone to tape before stretching to protect the fascia from re-injury. Too much stretching can re-injure the fascia and cause Achilles tendonitis. I would apply ice to the Achilles tendon after stretching if it begins to hurt. Injuring the Achilles tendon is serious for those with heel pain because it prevents future stretching. Applying ice to the calf muscle after stretching is recommended by some physical therapists to "preserve the elastic deformation" of the muscle (that is, it's supposed to retain the stretch better). During the first day or week of stretching, significant progress can be made. However, those who have had an inactive lifestyle or desk job may require a month of stretching to acquire a good level of flexibility. Stretching the hamstrings may also be important if there are sciatic nerve problems or a pelvic tilt is present. Below are pictures of stretching methods. The first, my favorite, uses a board placed on a brick. The second is against a wall, the third is Prostretch ($30), the fourth is a night splint ($60), the fifth is a wedge, and the last is the FootFlex ($30). Those devices that bend the toes back while stretching may take advantage of the "windlass mechanism" to keep the arch of the foot while stretching (see running section). I do not strongly recommend buying any stretching devices. Lack of flexibility in the calf muscles (a.k.a. ankle equinus) is the cause of many chronic cases (although simply being overweight is also a cause). The lack of flexibility continually places the plantar fascia under strain, continually re-injuring it. Simply following a stretching routine is not enough: being able to see an increase in the angle the feet can bend back after the first week if not the first day is important. I stretched for months using a mild approach and saw no improvement. I switched to a more aggressive routine and saw dramatic improvement. Muscles (not ligaments or tendons) lengthen while stretching, so the stretch should be felt in the calf muscles and NOT the first six inches above the back of the heel (in the Achilles tendon). Many sources say cold muscles should not be stretched, but stretching when first getting out of bed every morning is necessary to prevent re-injury due to lack of flexibility. The calf muscles and fascia can be warmed up in the morning (before walking and stretching) by using a heating pad and/or massaging device, but few will need to go this far. Stretching is more effective when the muscles are warm after activity. There may be benefit to stretching the fascia as well as the calf muscles. To stretch the calf muscles, leaning against a wall is popular. I stand on a 10"x8"x1" board with one end on top of a brick. This allows both legs to be stretched at the same time and the angle to be adjusted. I can see my progress by how far the brick can be placed under the board (which increases the angle). If progress cannot be seen, the overall amount of time spent stretching each day may need to be increased. A high level of flexibility has been achieved when one can stand straight on a 30 degree incline, but most people never achieve this angle. The average person can bend the foot back 20 degrees, but there is disagreement about this number and how it's measured and there is a wide range in the population. As a check to see how much improvement in stretching is needed, find a book or two, stack them on a hard surface, and place the balls of your feet on the edge of the books and lower your heels to the ground. Keep changing the book(s) until you find one (or a stack of two) that starts to barely allow you to stand straight and your heels barely touch the ground. Divide the height of the stack by the distance from the base of the stack to the back of your heel. Judging from the responses to our survey, I would keep up the stretching until the ratio is greater than one-third (0.333), which is 18 degrees. (Use the ATAN button on a calculator to calculate your angle from the ratio.)
A 30-degree angle is created when one edge of a 10-inch board is 5 inches above the ground. That is the angle of "wedges" used by physical therapists (I've seen three different designs use a 30-degree wedge). Some people have difficulty standing straight on a 15-degree incline, and yet they do not have heel pain. Others can stand straight on a 30-degree incline, and yet they still have heel pain (but I don't think they need to stretch and that they should not stretch because it may cause more harm to the fascia). I experienced a reduction in pain after stretching only a few days. Flexing the muscles while stretching. The technical name for this is Proprioneufacilitation (commonly known as PNF stretching). This method is faster than the plain "static" stretching described above, but it carries more risk of injuring the fascia and Achilles tendon. I usually apply tape when using this method to prevent injury. The balls of the feet can be placed on the edge of a step (or set of books) and the heels slowly lowered toward the step below, while concentrating on flexing the calf muscles, and holding this position for thirty seconds. If you place all your weight on one foot while doing this and concentrate on flexing the calf muscle, dramatic results can be seen, but it carries even more risk harm. This is the method I use, but it sometimes hurts my ankle. It may be that my foot bones are designed to bend back only so far and somehow that is causing the pain in my ankle. It's possible to see the calf muscles loosen up and the foot to bend back further in only fifteen seconds. The static method cannot achieve these quick results. I believe PNF stretching three times a day is the best method if the patient is sure it isn't harming the fascia. It can and sometimes should be repeated twice, three times a day. It feels good to sit down and massage the calf muscles in between stretches and may also help loosen them up. I usually use a combination of static and PNF stretching during the day. Night splints. I found 6 different journal article abstracts that reported success using a night splints. I did not view the entire articles of most of them and couldn't determine how long they should be worn. It's implied that they should be worn overnight but several visitors have reported harm by wearing them for too long. They were rated well in our survey and didn't appear to be any more harmful than most of the other treatments. The most common complaints are that they are too bulky to sleep in or that they snag on the sheets. I injured my Achilles tendon and heel (fascia) on two different occasions by leaving one on for only thirty minutes, three nights in a row. The more serious incident prevented good stretching for about six months and caused a serious setback. I would stop using them if there is any increase in pain in the foot or in the back of the lower leg. Ice should be applied afterwards to the fascia and Achilles tendon, especially if there is pain. A lower center of gravity (pregnancy, equipment belts, and "large hips") can cause plantar fasciitis because the foot has to bend back further before the center of gravity is able to pass over the toes. Better flexibility in the calf muscles is required for these cases. The fascia can be stretched by bending the toes and foot back for ten seconds, ten times each day, especially before getting out of bed or after long periods of sitting. It may reduce pain and allows injured tissue fibers to align properly while healing (or at least that's the theory). Improper tissue alignment while healing reduces the flexibility and strength of the tissue. One method is to hold two ends of a towel and gently pull the ball of the foot back for thirty seconds, with fifteen-second breaks, up to six times. One visitor writes: "I grasp my toes in my hand and pull the toes back while massaging the rear of the plantar fascia. I do a set of three, two or three times a day. This appears to work better than anything else I've tried." I would apply ice afterwards. A recent journal article claims stretching the fasia is more important that stretching the calf muscles. Toe and Foot Muscle StrengtheningStrong foot muscles promote better overall functioning of the foot and thereby can help take some of the tension out of the fascia. There is a theory that always wearing shoes and sitting at desk jobs have allowed these muscles and tendons to atrophy. Laying a towel on the floor and pulling it back using only the toes is often prescribed by physical therapy. Another technique is to place the feet flat on the floor while sitting in a chair and pushing the ball of the foot off the floor by pushing down with the toes. Another method is to pick up marbles or similar objects and place them in a cup. Pressing the toes on the ground while walking may noticeably reduce pain in the heel because it takes some of the tension out of the fascia and places it in the tendons that pull the toes down. MassageFrequent massage of the fascia, as often as possible and especially in the morning, increases fluid flow in the area, which may speed healing. Vigorous, deep massage of the fascia may also help by breaking up scar tissue. Often, a lump of scar tissue can be felt and broken up with very deep and hard massaging (but if it's cancer, breaking it up would help spread the cancer). Eighteen percent of 290 of our visitors who tried deep massage report that it caused them harm. This is a high percentage so I can't recommend it, but I would most definitely apply ice before and after if I tried it. Once the scar tissue is broken up, stretching the fascia by bending the toes back for ten seconds, ten times each day, may allow the tissue to heal back stronger and more resilient. Vigorous massage to break up scar tissue before getting an injection has also been recommended. Some have emailed to say their plantar fasciitis was cured after they were forced to run and then the pain subsequently disappeared. Whichever method is used (deep massage, rolling pin, or running), I would apply ice immediately afterwards and try to keep it cool with ice for several hours (but not so cold that it's painful). TapingThe following is long-winded.Our best document on taping for easy printing is athttps://heelspurs.com/tape.html Athletic tape can help speed healing by protecting the fascia from re-injury (especially during stretching). It can be thought of as a way to give the fascia rest without decreasing activity. In severe cases, it can enable the patient to walk again. Tape is used to supplement or replace the function of the fascia. Tension in the tape replaces tension in the fascia. If the tape is tight when standing and walking, and the pain is not immediately relieved, then tension in the fascia is probably not the cause of the pain. You can find good athletic tape at CVS and Rite Aid. I applied tape every day for three years. Before taping, my ability to walk was severely limited. I took it off every night at bedtime to allow the skin to breathe, dry, and heal. Taping may harm the Achilles tendon because it decreases flexibility in the foot, which would require the Achilles tendon and calf muscles to stretch farther than normal. Firm (not soft) heel pads can help prevent Achilles tendon damage when using tape by compensating for the loss of flexibility, but as discussed elsewhere, dependency on the pad can develop. When removing tape, skin can and will peel off, especially if the skin got moist while wearing the tape. It is probably more likely to happen to those who are older and overweight. It is a serious problem and I do not know of a remedy. I had to stop applying tape one time because of the damage to skin. Now for an interlude from the email bag..... "Being a Registered Nurse and spending a lot of time in First aid/ sports injury type suitations I have found that application of friars balsam (tinc benz co) is very usefull at protecting skin a simple application with a swab over the skin to be taped giving it a few minutes to dry will radicaly reduce the problem of damaging the skin." Doctors sometimes apply tape and advise to leave it on for too long (in my opinion). Tape appears to lose most of its effectiveness after less than a day and begins to reek if it gets wet and is left on for days as many doctors recommend. All the methods I've seen lose most of their effectiveness after thirty minutes of walking but can often provide some protection for up to a full day. If the tape loses its effectiveness during the day by stretching or slipping, I add another layer of tape to take away the slack. Washing the foot with soap and water first is usually necessary for the tape to stick. Washing with soft water may make it difficult for the tape to stick; therefore using bottled water may be necessary in some areas. Visitors have said hair spay may help it stick better. Visitors have also said there are other sprays available (like Tuff-Skin) that may help it stick but they seem to be hard to find (and spay cannisters have shipping problems). Applying Maalox and then letting it dry before applying tape has been said to prevent the tape from causing the skin to peel. The first two strips of tape in the picture below shows my favorite method. This saved my ability to walk. I sometimes added a 3rd piece as shown. Even with the slack in the tape this method is very helpful because it decreases the tension in the fascia when it is at its greatest. Arch support can also decrease the slack because it makes the tape travel a farther distance, so using tape with arch support may be a good or excellent idea. If the tape has no slack it usually caused my ankle to hurt.  To see the really big pictures of my favorite taping method, click here When I walked a lot, I had to add more layers during the day. Duct tape is a good additional layer because it is less expensive. Using athletic tape for the additional layers may cost as much as $1 a day. Tape that has no slack in it may cause too much pain in other areas. If I applied it too tightly or improperly, it started to hurt my ankle, foot, and knee while walking. If it was not tight enough, my heel started hurting again. It took a lot of practice to get it where it helped the fascia but didn't hurt other areas. The objective was to keep tension in the tape instead of the fascia when standing and walking. When the heel pain was great, I would minimize the amount of slack if it didn't cause too much pain in other areas. Just because a doctor applied the tape, it does not mean the tape was applied correctly. Doctors will often say that if tape helps then an orthotic will help, but I think it's a dubious claim in one sense ("low-dye taping prevents pronation similar to an orthotic") and clearly wrong in another. Orthotics cannot reduce tension in the fascia like the way I tape. A a thin strip of skin would sometimes peel off when taking the tape off, especially if the skin had become moist during the day. I found the best way to peel the tape off was to start at the ball of the foot and peel slowly and very carefully. I often applied duct tape directly to the skin, but a certain extra-strong red type that must have used a different glue caused the skin to peel off. It was fairly serious. However, most duct tape stuck better than athletic tape so that I sometimes applied duct tape first and then a layer or two of athletic tape. Duct tape, even several layers, had the problem of stretching out. Athletic tape did not appear to stretch). One visitor wrote to say that hockey tape is safer for sensitive skin, but "hockey tape" and "athletic tape" are often referring to the same thing. There is also hypo-allergenic athletic tape. There are other ways to tape, but whatever method is used it should connect the ball to the heel in order to work (there is a "low-dye" method that doctors often use, but I didn't find it useful and I don't have pictures of it). The pictures below show a slightly different approach. Bending the foot back (dorsiflexion) when placing tape on the back of the heel helps because it prevents the skin from getting pulled when walking. The skin on the back of the heel will try to stretch when walking and bending the foot back before taping will cause the skin to give itself some slack ahead of time.
Arch Support and Medial Wedges (Posts)Better shoes, inserts, or orthotics (also called orthosis when singular, orthoses when plural, and orthodics when misspelled) can provide arch support. Arch support is indispensable for many if not most cases. However, too much arch support can cause the fascia to stretch a longer distance. This causes it to pull harder at its attachment to the heel, causing pain over the short-term and a repetitive injury over the long-term. Arch support that is too high and close to the heel can pull the fascia directly from the heel. Those with flat feet may benefit more from arch support. Those who over-pronate (their inside ankle bone rolls down and inward too much when walking) may wear out their shoes on the bottom on the medial side (medial = inside on the side next to the other foot) and may need new shoes. Over-pronators may need (in addition to arch support) a "medial wedge" or "medial post" or "varus post" (an angled support that is higher on the medial side than the lateral side). The lateral side is the outside edge of the foot - the opposite of the medial side. Two wedges have been recommended by at least one source, one under the fore foot (ball) and one under the rear foot (heel bone) which are about 2 to 7 mm thick on the medial side. Many health care professionals who readily mold and charge for an orthotic are not aware of this technique. I would ask if I over-pronate, and if I did, I would ask if I needed a "medial post or wedge." Shoes with wide or flared heels increase pronation. A high arch may also benefit from arch support and maybe a lateral wedge under the fore foot. Powersteps are good arch supports for $24. If you use heel pads under inserts and have a high arch, you may need New Balance running shoes because they are one of the few brands that come in wide sizes. Custom orthotics are inserts designed from a mold of your foot. Seventy percent of patients in a study reported improvement with custom orthotics, which is as high a percentage as stretching. This study has been criticized for using only "rigid" orthotics, when semi-rigid orthotics are more commonly used. Orthotics cost between $100 and $800 a pair, depending on how large a profit margin the doctor or orthotics maker is trying to make. A doctor's prescription is often necessary for orthotics. Physical therapists may also make a mold of your foot and send off for orthotics. InjectionsCorticosteroid injections are often used to reduce pain and inflammation. It is a controversial topic among doctors. Some studies, many doctors, and patients report a lot of success with shots. Our visitors ranked shots fairly high as a treatment, but some studies and doctors strongly advise against shots because they slow down the healing process, can cause the fascia to detach (one doctor said he doesn't see much of a problem with that because that's what surgery does), and causes the fat pad to deteriorate, causing long-term damage. One study reports that ten percent of the injections they applied resulted in plantar fascia rupture.23 The relief is often only temporary. Of our survey respondents, thirty-five to fifty percent have had shots. Shots will mask the pain, so it may not be wise to jump back into activity. There are "water-soluble" (a.k.a. soluble) and "fat-soluble" (a.k.a. insoluble) cortisones. The insoluble type stays in the tissue longer, thereby causing more tissue damage (but more pain relief). The soluble type is fast-acting but temporary. Vigorous massage to break up scar tissue before getting an injection has been suggested, but if there is significant pain to the touch, I wouldn't try it. Shots themselves may help break up scar tissue by deteriorating the tissue. This may help pave the way for better healing. Shots are often very painful if the doctor is not caring or knowledgeable enough to minimize the patient's pain. Maybe there are some cases where it can't be done painlessly. The phrase "worse than childbirth" is sometimes used to describe it, but 25% of the time the pain is minimal. One source says that in order to reduce the pain when injecting, a medial approach using a long and small diameter needle and local anesthesia is necessary. It is interesting to note that according to our surveys, orthopedic surgeons are half as likely as podiatrists to give injections, but they are nearly twice as likely to be very painful when given.
Dr. Zuckerman writes:
John H summarizes a Runner's World article:
Fifty percent of our visitors who had shots said the pain was "pretty bad" or "horrific." The other fifty percent said they were "not too bad." Some doctors will give shots before resorting to a cast or surgery. It is very rare (if not illegal) for doctors to give more than three shots in a year because of the dangers. Two shots is considered a maximum by some. On separate occasions, I have heard of doctors giving roughly twenty shots for heel pain. I have not been able to figure out "what's up with that." Shots are not considered "conservative" therapy. Reducing the InflammationInflammation in the heel area (even though it may not be visible) can increase the amount of heel pain for twenty-four hours a day. Elevating the heel as high above the heart as possible for as long as possible can help. Sleeping on the stomach with the foot on top of two pillows may help, as will placing the feet up on a desk. A difference may be noticed in only fifteen minutes, but when my inflammation was severe, it took several hours for several days in a row to see noticeable improvement, which was very much welcomed. Compression can be very helpful. For example, I've found stepping on the edge of a step or thick book so that the heel area is compressed for two minutes reduces the pain for an hour or two. Compression squeezes fluid build up out of the tissue, and it takes an hour or two for the fluid to build up again. Injections reduce inflammation as discussed above and nutritional supplements are beneficial as discussed in the next section, but doctors commonly prescribed medication as discussed below. Anti-inflammatory medication: Ibuprofen gels and creams may be the best and safest (I'm not aware of an FDA study but some formulations have worked great on me), but they are often hard to obtain in the U.S. Ibuprofen and aspirin pills may help. Inexpensive prescription pills include Naprosyn (naproxen) (same as over-the-counter Aleve except in a double-strength dose), Daypro (oxaprozin), or a corticosteroid such as Deltasone (prednisone). I've experienced the greatest benefits from prednisone, but it carries the most risk. The maximum prescription doses of ibuprofen (Advil, Motrin) are four pills (200 mg each) four times a day (twelve per day), but rxlist.com says it was not much more effective than three pills four times a day. I would not take that much ibuprofen unless I had to and not for more than a few weeks if I did. I like having intestines, kidneys, and a liver that function properly. Taking ibuprofen and other NSAIDs with food and water is highly recommended because of the intestinal and stomach damage they cause. Ibuprofen is supposed to be safer for the digestive system than aspirin, but more dangerous to the kidneys. Long-term use of anti-inflammatory medications kills 7,000 (or it is 16,000?) people each year. Be sure to read the dangers associated with your particular NSAID, such as not drinking alcohol, staying out of the sun, and interactions with other blood thinners. Aspirin and Ibuprofen are good NSAIDs, but Tylenol does not reduce inflammation because it is not an NSAID. Tylenol has the lowest success rating in our survey. Vitamins and Nutritional SupplementsWe have been exposed to a variety of natural compounds in the environment for millions of years and have evolved to tolerate their presence. They are rarely harmful when ingested and rarely interact with other compounds. Many of them are beneficial for many ailments. Unfortunately, we are generally unaware of their beneficial characteristics because they cannot be patented. Patents enable large profits that support researchers, advertising, vacation-conferences for doctors, and a network of drug representatives. By definition, patentable compounds are recent designs. As a result, we have not evolved to cope with them and they are always toxic and have complex interactions with each other. According to JAMA, about 106,000 people a year die from doctor-prescribed medications when taken as directed. This makes prescriptions the fourth or fifth leading cause of death in the U.S. It has been estimated that 16 people die each year from supplements. If people are taking as many supplements as drugs, that means drugs are 6,600 times more toxic than supplements. But just because supplements are safe, it does not mean they are less beneficial. Pharmaceutical companies can find a natural compound that safely and inexpensively helps a specific health condition and then modify its chemical structure into something that can be patented and sold. The result is a compound that works more or less as well as the original supplement and is always toxic. We have evolved to tolerate compounds made by fellow DNA-based organisms that operate in low-temperature, low-pressure conditions. This is very different from compounds made in laboratories. Insulin, penicillin, morphine, and aspirin are some of the few champions in the field of medicine, but they're all natural compounds designed and made by DNA before Mr. Merck was a twinkle in his father's eye (the 1600's). Patentable compounds have a beneficial side effect to the medical community: their toxicity necessitates a doctor's prescription. Nurses are usually much more knowledgeable than doctors about supplements because their profession has not been supported and influenced by pharmaceutical drug companies. Since nurses cannot write prescriptions, their schools and conferences do not need to be influenced by the toxic drug money. If you mentioned a nutritional supplement to a doctor in the 1970's he would have said "Huh?". In the 1980's doctors said with authority that supplements are harmful (eventhough they wouldn't know anything about them). In the 1990's doctors said supplements were useless but they probably wouldn't hurt you. Now they are acknowledging that there are some benefits, and some might even recommend calcium (eventhough you need vitamin D more than calcium - and more nurses than doctors know what I'm talking about). In the year 2020, I believe doctors will finally be as knowledgeable about supplements as nurses were in the 1970's. This is not an exaggeration or joke, but a very serious situation that has caused the death and misery of millions. As a measure of the toxic drug money influence, the Journal of the American Medical Association (JAMA) had 135 pages of pharmaceutical advertisements in an issue that stated "It has been estimated that $8,000 to $13,000 is spent per year on each physician [by pharmaceutical companies]."1,2 There was not a single advertisement or mention in that issue for any of the nutritional supplments that cut the risk of cancer in half - something no pharmaceutical drug has ever been able to accomplish despite billions in research. And most doctors cannot name those supplements eventhough they can name many useless chemotherapy poisons. By far the best nutritional supplement books I've seen (I've bought thirty-two) are by Michael T. Murray. His best overall book is Encyclopedia of Encyclopedia of Natural Medicine (1,000 pages and 2,000 references). Most of the information in the next three paragraphs comes from his books. Vitamin Shoppe has OK prices and excellent quality. They have a great catalog. Call 1-800-223-1216 for a catalog. www.nutriteam.com has great prices if they have the product you are looking for. WalMart has the least expensive vitamin C. Supplements can be placed in a small hand-held fisherman's tackle box so that bottles do not have to be opened. I do not mind taking lots of them because supplements are more like food than drugs. Supplements that reduce inflammation: Over-the-counter and doctor-prescribed anti-inflammation medications are harmful as discussed in the "reducing the Inflammation" section. Safer alternatives are (in the order of my favorite choices): The following two supplements often have an effect in an hour and will last for several hours. Pancreatic enzymes three times a day with food. This decreases appetite in addition to reducing inflammation. Bromelain (pineapple extract) is another great reducer of inflammation; 1,000 mg (which is approximately equivalent to 4,000 GDU or 6,000 MCU) with grapefruit juice or on an empty stomach will increase absorption. I've had the most dramatic results in 10 minutes with DMSO. Two tablespoons a day of flax oil (an Omega-3 source) is supposed to reduce inflammation. Flax oil is difficult to prepare properly and spoils easily. Many brands are ineffective, but the Barlean brand from Vitamin Shoppe is reputable. Eliminating animal fat except for mackeral, albacore tuna, salmon, herring, and sardines (all of which include Omega-3 and other beneficial fats) is supposed to reduce inflammation. Eliminating polyunsaturated vegetable oils and trans-fatty acids, such as margarine and partially hydrogenated vegetable oils, is also supposed to help. Increasing the consumption of good fats and decreasing the harmful fats in the diet is very beneficial to overall health. Quercetin is supposed to reduce inflammation. Dr. Andrew Weil says, "To reduce inflammation, take two 500 mg capsules of powdered ginger once or twice a day with food, or one 400 to 600 mg capsule of curcumin (obtained from the spice tumeric) three times a day." I have used half a teaspoon of ginger to make hot ginger tea and saw drammatic improvement in an hour or two. Heel and general foot pain may sometimes be a symptom of ARTHRITIS, especially if there is arthritic back pain and it's in both feet. For all forms of arthritis, I would try 1 gram of niacinamide 3 or 4 times per day, 1 to 4 grams of vitamin C 4 times a day (if it doesn't cause an upset stomach), bromelain, flax oil (see above paragraph), capsaicin (the topically-applied pepper compound), pancreatin, and 100 mg vitamin B6. For osteoarthritis, I would try 1,500 mg glucosamine sulfate each day before anything else. For rheumatoid arthritis, I would try vitamin B5 and adrenal cortex extract in addition to the others mentioned above. According to Michael Murray's references, chondroitin and shark cartilage does no more than glucosamine and are not needed. Less than 8% of chondroitin is absorbed and it is merely a less-refined form of glucosamine. Supplements to increase tissue strength: The following supplements may have anywhere from no effect to a large effect. I use them because they do no harm: At least 1,000 mg vitamin C with each meal and before bedtime. This may help tissue heal back stronger, but it is more likely to be beneficial reducing pain and stress (both mental and physical). The only person to win two Nobel prizes unassisted (Linus Pauling) estimated that people would have, on average, twenty-five extra years of good health if they took the optimum amount of vitamin C (which he estimated to be between 2,300 and 10,000 mg per day). If you get a cold or cancer, 500 mg to 1,000 mg can be safely taken every hour (if it doesn't cause too much gas and diarrhea). Sodium ascorbate and calcium ascorbate do not cause the gas and diarrhea that may occur in the more common acid version of vitamin C, ascorbic acid (aka hydrogen ascorbate). It's the ascorbate ion in these compounds that is the actual vitamin C. I have not read of any specific cases where it has happened, but greater than 4,000 mg per day may cause those who are sensitive to oxalic foods like spinach to get kidney stones. Other supplements supposedly good for tissue strength: 2 mg copper and 15 mg zinc. Manganese (not magnesium) 50 mg four times a day the first two weeks, then 20 mg day, is supposed to increase SOD levels, which speeds healing. Europeans can get SOD injections. Grape seed extract 60 mg twice a day is supposed to prevent collagen destruction. I would choose the source of grape seed extract carefully (www.nutriteam.com seems good). Zoloft is one of the best anti-depressants that works for the largest number of people. Less effective over-the-counter pills are 5-HTP, St. John's Wort, and Kava (Vitamin Shoppe brand only -- herbs from many brands are notoriously ineffective). Kava is best to relieve stressful times. It's mainly a muscle-relaxant. DHEA is a precursor of several hormones that most everybody over 40 should probably be taking. It usually makes you feel and sleep better, increases the libido, increases bone density, and improves the muscle to fat ratio. The dosage is 10 to 50 mg per day. One 50 mg dose improves my sense of well-being, energy levels, sleep, and libido for two days, but if I take it every day I get jittery. I'm 35 years old. Friends who are also in their 30s have confirmed some of these effects. A recent journal article indicates testosterone therapy decreases the incidence of prostate cancer eventhough it has been speculated for many years that it may increase the risk. Hopefully DHEA would also decrease the risk, but i do not yet know of any studies that show it increases or decreases the risk. To quote one article "using DHEA in order to cure sexual troubles might be considered, although the possible negative effects of DHEA, especially on breast and prostate, have not been discarded yet." (Gynecol Obstet Fertil. 2002 Dec;30(12):961-9. ) Concerning breast cancer, another article stated "DHEA also inhibits the growth of human breast cancer ZR-75-1 xenografts in nude mice. The inhibitory effect of DHEA on breast cancer is due to an androgenic effect of testosterone and dihydrotestosterone made locally from DHEA." (Front Neuroendocrinol. 2001 Jul;22(3):185-212) I hesitate to mention the following because it may increase the incidence of prostate and breast cancer and a journal article reports it has no effect. It's used by a lot of older men to increase energy and libido, and by weight-lifters. Androstenedione (a testosterone precursor) and other over-the-counter testosterone boosters may increase the rate of tissue repair. Possible side effects include happiness, increased aggression, deepening of voice, acne, prostate problems including cancer, male hair loss, masculization effects in women such as more hair on the lip and face, extra muscle mass when combined with workouts, and weight increase (due to muscle). The Nor-andro products are supposed to not have the negative effects, but I'm wary of them because they are not pure testosterone precursors (they produce fake testosterone) and may cause liver damage or prostate cancer (but I've not read anywhere that they do). Several people have claimed MSM helps, and a friend swears massive amounts of vitamin B1 cured his heel pain. Heel PadsOur visitors report that heel pads are not the most effective treatment, but it's important to go into detail about the theory behind their use because it explains a lot about the mysterious causes of heel pain for those who are not overweight. I have personally been helped a great deal by heel pads, but I may have also been harmed somewhat by them by developing a dependency. Heel pads can be used to alleviate two different dysfunctions. If the heel is sensitive to the touch or if the fat pad under the heel is thin from age, disease, excessive use on hard surfaces, or too much weight, a soft heel pad can be used to protect the heel. I call soft types of heel pads "heel cushions." I refer to a heel pad as a "heel lift" when it is firm or hard. The primary purpose of a heel lift for those with heel pain is to raise the heel to make up for a lack of flexibility in the calf muscles. Heel lifts are also used to make up for having one leg 1/4 inch or more shorter than the other. Making up for one leg being shorter improves gait which may also prevent damage over the years to the hip socket or back. Heel cushions are usually just placed in the back of the shoe, but not placing them under the shoe insert or orthotic will reduce the effect of the arch support, if there is arch support. Heel lifts are usually placed under the shoe insert (if the shoe has one) or orthotic.A heel cushion that is still thick when compressed under body weight is also functioning as a heel lift. I call it a "heel pad" if it's serving both purposes or if I'm referring to the devices in general. Using heel lifts or heel cushions that are 1/2 inch; thick when compressed increases the effective ability of the foot to dorsiflex by about 5 degrees. If placing 1/2 inch of carefully folded paper (to simulate a heel lift) under the heel immediately relieves pain, stretching the calf muscles without re-injuring the fascia is probably needed. The phrase "heel cup" describes those designs that have sort of a pocket for the heel to fit in. They are meant to help the heel fit more snugly above the cushion. They usually have a waffle-like plastic or rubber design on the bottom. The waffle design makes the plastic or rubber softer when placed under pressure. Heel cups usually function as a good heel cushion but do not usually have much thickness during compression so that they may not function very well as a heel lift.Heel pads are needed in both shoes so that problems in the back, hip, legs, ankles, and feet do not result from uneven leg length. If there is a lack of flexibility in the calf muscles, walking barefoot without heel pads can be harmful. This is especially true on hard surfaces, not just because they are hard, but because cushioned surfaces "give" and "place a spring in your step" in such a way that it makes up for a lack of flexibility in the calf muscles. (now I'll digress to explain this effect in detail) When walking on soft surfaces, body weight shifts from the heel to the ball, which causes the front of the foot to push lower into the cushioned surface. At the same time as the ball of the foot is pushing down, the heel is experiencing a small upward push from the floor which is trying to regain the shape it had before it was placed under the weight of the heel. This pushing downward in the front and upward at the back occurs at the moment of maximum tension in the plantar fascia, but it reduces that maximum tension because the soft surface has allowed the foot to be at an angle downward and the net effect is as if a heel lift were in place. The effect is especially important for those who have a lack of flexibility in the calf muscles. The moment of maximum tension is when the heel begins to come off the ground and is called "heel off" in the gait cycle. In short, soft surfaces function similarly to heel pads in how they provide cushion and compensate for lack of flexibility in the calf muscles. The combination of hard surfaces and lack of flexibility in the calf muscles appears to greatly increase tension in the fascia. Two visitors have emailed to say switching from carpet to hardwood floors was the beginning of their heel pain. Getting up every morning and walking barefoot on a hard surface when the feet have not been warmed could cause re-injury each day. Turning the front of the foot inward toward the other foot while walking and walking on the outside edges of the feet lessens the strain on the fascia and can be helpful for those early morning steps and middle-of-the-night excursions. (Warning: a reader emailed to say he developed a habit of placing his weight on the outside edge of his foot. It resulted in a collapsed cubiod bone.) Religiously wearing soft-soled shoes before walking anywhere on hard surfaces may be wise, and many businesses know that floor mats can be a life-saver to their employees' feet. Most heel cushions are less than 1/4" thick when compressed. Good, thick heel pads are hard to find. Folded paper placed under thin heel cushions can be used to raise them higher. Using heel lifts while playing sports such as tennis greatly increases the chances of severely injuring an ankle during a turn or a stop sideways. I tried to continue a calf muscle stretching program while wearing heel lifts so that a dependency did not develop. CastsA study reports sixty-three percent of their forty patients who wore a cast reported mild to excellent success. Four to six weeks in a cast forces rest and neutral stretching. Doctors may be predisposed to trying casts because it is one of the few treatments they can try. But an older article (Callison Orthopaedic Foot Club Meeting 1989) said sixty-one percent of patients had recurrent pain within four weeks of cast removal. Visitors have emailed to say that casts made their condition worse and they had to be removed in a few days because of the increase in pain. There are removable casts available from some doctors that are an excellent alternative. Doctors or physical therapists can make a cast that is open on the top so that patients can strap their foot and ankle inside using ace bandage. Some night splints can be used as a substitute for casts and can be removed, so they may be better. SurgeryMost surgeries will be replaced by ESWT because ESWT is safer and appears to have a higher success rate. In short, if a friend asks if they should get surgery for heel pain, I answer NO. Now here's the long story... 8% of our visitors have had surgery with a self-reported success rate of 37% to 60% depending on the type of surgery. About 20% have reported that surgery has made their condition worse. These results are much worse than what is reported in most journal articles, but closer to what some doctors are tell me by email. It may take 6 months, a year, or never for the damage done by surgery to heal before improvement can be seen. Our results may be much lower than what journals report because journal articles are about ideal cases performed by the best doctors. If our visitors do not have the same set of symptoms, then the surgery being studied in any particular journal article would be less comparable to our results. Out of necessity, doctors may be applying the various surgeries to a wider range of cases than was intended in the journal articles. Those publishing the studies are often those that have the most experience and skill in that type of surgery. Other doctors may not implement the surgery in the same way. Another possibility is that patients and doctors have different ideas as to what constitutes a successful surgery. A 4th possibility is that patients overestimate the success of a surgery when speaking to their surgeon. In journal articles surgery is reported to have a success rate of 50% 17 to 97% 22, et al, depending on which source is quoted, which surgery is used, and on which doctor performs it. Endoscopic plantar fasciotomy (EPF) is the newest method. Other surgical techniques are still more common and require a larger incision (up to two inches) that takes longer to heal (after reading the message boards, I get the impression six weeks to a year is required, or forever), but some doctors may prefer the older methods to endoscopic plantar fasciotomy because these methods allow them to see better and cut more accurately (and possibly to relieve nerve entrapment or remove the spur). There is also a "minimal incision" type of surgery that may be as beneficial as EPF and not as dangerous as other surgeries that require larger incisions. Several sources say surgery is ultimately required in about ten percent of the cases, but many doctors claim it is needed in less than five percent of their patients. Most doctors require conservative treatment (which means no surgery, and usually it means no shots) for about twelve months before considering it. When I say "doctors" I'm lumping podiatrists and orthopedic surgeons into the same category which requires a very ACTIVE imagination. Endoscopic plantar fasciotomy is relatively new and requires equipment and skill that some doctors do not have. Some surgeons do not think it is more effective than other types of surgery, but there is at least one journal article that indicates otherwise. Our visitors do not rank it as well as heel spur removal surgeries, but the results are not statistically significant. It was first performed around 1991. From our surgery database and journal articles, it appears that podiatrists are using it much more often than orthopedic surgeons (it appears to have been developed and/or researched by podiatrists). The procedure takes twenty minutes to an hour and does not require a stay in the hospital. The surgeon detaches (cuts) a portion of the plantar fascia from the heel. A slotted tube is inserted through two small incisions (less than 1/2") in the skin on each side of the heel. Sometimes an incision is made only on the inside of the heel. An L-shaped knife inserted down the tube pokes out of the slot, cutting the fascia as the doctor rakes the knife back and forth. An endoscopic camera is inserted into the tube to allow the surgeon to see what he is cutting (this is the origin of the "endoscopic" portion of the EPF name). The cut fascia usually relieves pain and pressure in the area and new fascia tissue grows into the gap created by the cut. Practice on cadavers is necessary during training. The two-portal (two incisions) method was patented by Dr. Barrett in 1993. Dr. Barrett says, "Most patients return to their regular shoes in 3-5 days. Most return to work after the first week, and return to their normal activities by the end of the third week. Everyone heals slightly differently. Other factors such as age, weight, and occupation can contribute to healing times." In a 1995 J Foot Ankle Surg report, Dr. Barrett reported that one month was the average time required to return to work. This report indicated open heel surgery was not as effective. Footlaw.com states cuboid pain, nerve entrapment, severe arch discomfort, and post-traumatic nerve syndrome are all potentially serious complications of EPF (and possibly other fascia release surgeries), although it also states that many patients are helped by the procedure. A November 2005 message board post on EPF Surgery by a footlaw.com lawyer does not speak highly of EPF. The pictures below are what doctors see on a TV monitor when doing EPF. 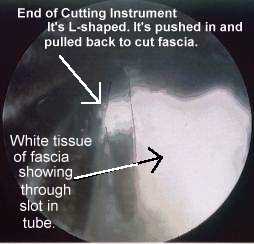  An orthopedic surgeon informed me that he saw about 500 cases of plantar fasciitis (heel spur) in two years. Fifty percent of his patients get better with better shoes, rest, NSAIDs, frequent massage, ice, and stretching. He subjects the other fifty percent to shots. So out of every ten patients, five get the shots. Three of those five are cured with the first shot. The other two get the second shot. One of those is cured. The last one (out of the initial ten), 10% gets EPF surgery. He reports only one or two surgery failures out of fifty. After the surgery, patients are walking the same day without pain (this is rare, compared to visitors who post to this site). In four weeks their activities are back to normal without pain. He no longer performs surgery on both feet at the same time. EPF and other surgeries that release the fascia usually cut only the portion of the fascia over the inside front of the heel bone where the bone sticks out a little to connect to the fascia (a.k.a. medial calcaneal tubercle). In the past, detaching the entire fascia was more common but there were more frequent complications. Whether non-EPF fascia release surgeries are more or less effective than EPF is debatable. I believe EPF is more effective, unless a particular doctor has perfected a minimal incision method. I do not think detaching the entire fascia from the heel would be wise in the majority of cases because of the fascia's important role in connecting the heel to the ball of the foot and thereby creating the arch in the bone structure of the foot. Complications for fascia release surgeries: The arch may fall some or have other problems after fascia release type surgeries (including EPF). Using arch support after surgery is recommended by some to help prevent the complications that result from a lowering of the arch. One journal article says surgery in those with flat feet may not be good (the exact quote is: "The data suggest that operations involving fasciotomy affect arch stability and should not be performed in patients with evidence of concomitant pes planus deformity, because of the likelihood of further deformation"). The Wheeless' Orthopedic web site says plantar fascia release (not nerve entrapment surgery or heel spur removal) "would appear to be an illogical procedure in patients w/ pes planus (flat feet)." The arch may drop some or other foot problems may result in addition to not curing the original problem. For example, I've had several visitors tell me the outside (lateral) edge of their foot started hurting after the surgery. If the pain is near the bottom and outside edge of the foot, it could be because more tension is in the lateral band of the fascia. If the pain is on the top and outside edge of the foot above or in the arch, it could be due to increased pressure between bones in the cuboid bone area caused by the lowering of the arch (the bones are changing their positions relative to each which may also stretch ligaments). Paper number 184 at the 1996 Annual Meeting of the American Academy of Orthopaedic Surgeons indicated the lateral side (outside edge) of the arch of the foot dropped 2.6 mm when only the medial band of the fascia was cut and that this was a possible cause of lateral arch pain after surgery (a joint and ligament on the lateral edge are experiencing more stress). The medial side of the arch dropped 4 mm. Here's a recent journal article's conclusion about fascia release surgery: Although plantar fasciotomies continue to be used to relieve the heel pain associated with plantar fasciitis, there are no criteria as to the amount of fascia release required to relieve symptoms while maintaining the integrity of foot function. .... The study demonstrated that partially releasing the plantar fascia imparts forces to the remaining fascia that are not usually observed with the fascia intact. .... When the plantar fascia was released, the subtalar joint was unable to resupinate in late midstance and propulsion, and there seems to be a direct correlation between the amount of fascia transected and the subtalar joint’s inability to resupinate. .... More research is needed to determine more precisely the amount of plantar fascia that can be released before significant increases in forces in the remaining fascia are observed and before loss of the subtalar joint’s ability to resupinate during late stance and propulsion. From this initial study, it seems that less than 66% of the fascia should be released to maintain foot stability, which is in agreement with in vivo research on lateral column symptoms following plantar fascial release. - Erin D. Ward, DPM et al, Journal of the American Podiatric Medical Association, Vol 93 #6 429-442 2003 Heel spur removal surgery (a.k.a. inferior calcaneal exostectomy) is often used, but some sources since 1990 indicate they should not be removed. According to Doctor Lundeen (www.drlundeen.com), "Beware if a surgeon says the spur needs to be removed...." A journal article says, "Radiographically [by x-ray] it was noted that, despite complete excision, subcalcaneal exostoses [heel spur] often reformed ... findings of this study suggest that changes within the fascia, rather than the spur, are primarily responsible for the pathogenesis of the syndrome." And "not in any case the calcaneal [heel] spur found [by X-ray] induces pain or tenderness. ... Results of the surgical removal of the painful calcaneal heel spur have been disappointing. ... Since chiselling down the calcaneal [heel] spur also removes the attachment of the plantar aponeurosis [fascia], patients must accept subsequent lowering of the arch of the foot." Another journal article abstract: "Four patients developed calcaneal fractures while walking, soon after bone removal from the under-surface of the calcaneus. Heel spur or osteomyelitic bone removal can lead to this complication." Should heel spur be removed? I don't know. Our visitors rank heel spur removal better than the other surgeries. A visitor emailed to say his doctor performs 150 heel spur removals a year "without cutting the fascia" with apparently good success (although the fascia may get partially severed out of necessity to reach the spur).  I do not know anything about surgeries directed toward nerves to relieve pain due to nerve "entrapment" or "involvement" and cannot comment, except to say that they ranked the worst among the surgeries reported by our visitors. In any surgery, a nerve may be cut during surgery (or inflammation from surgery may put pressure on the nerve) and cause pain, loss of sensation, and/or tingling in the bottom of the foot or in the toes. The doctor may call it "peripheral neuropathy." It is not necessarily permanent damage. Surgery may also injure arteries and veins that allow good blood supply and thereby increase healing time or cause deadening of tissue. This may be called "avascular necrosis." Click here to see nerves seperated from a human foot.
Immediately after surgery I would apply ice as much as possible for two days in order to keep the injury cool and to help it heal faster and stronger. I would also take it very easy (rest the feet) before slowly increasing activity in the absence of pain and listen carefully to the doctor's instructions. I would seriously consider arch support and tape, but tape if I chose only one of the two. Vitamin C is important for scar tissue to heal back strong. It is required in several of the steps in collagen formation; 4,000 mg spread out over each day may help if taken for at least a few days following surgery, but preferably for weeks. It used to be used in conjunction with all surgeries in the 1950s. For more information see my vitamin C rant. What to expect from surgery written by a patient Message from a patient about the VA's position on Surgery: I went to my local veterans hospital podiatrist yesterday. She told me that the VA just does not do PF surgery anymore since half the patients got better and half got worse. They got tired of the grief and letters to congressmen. Also, it they make you worse they have to pay compensation. What this tells me is that the surgery is risky because VA hates to pay claims for failed surgery. She said except for the most serious cases [where the patient cannot walk] they just did not do the surgery. OtherThese are methods of which I have only recently become aware or consider questionable. Prolotherapy is a series of injections that are supposed to speed healing of ligament tissue (fascia is similar to ligament). See www.prolotherapy.com for more information. Ionotophoresis consists of applying current through electrode pads placed on the skin which are covered with a gel or solution of steroids or other chemical. The current carries the chemical through the skin. The current itself may also help. You may see this at your physical therapist's office. A study reports that Ionotophoresis six times for two weeks helped some, but there did not seem to be a lasting effect after one month. Pedorthists are shoe and orthotic specialists. Acupuncture, magnetic inserts (or a magnet at the painful spot -- Radio Shack has special, very strong, very small magnets that you can tape to your heel), and chiropractors have been used. I've used a set of twelve "Rare Earth" magnets from Radio Shack in a grid pattern (but you have to make sure the polarity is the same or they cancel each other out: place them in a stack sticking together and then slide them off one at a time and place them in a duct tape sandwich without the little magnet disks flipping over - it isn't easy because they are so small and so powerful that they are very difficult hard to handle.) Psychological/Social IssuesNot being able to walk as much as you would like can cause a great deal of psychological pain. This is often compounded by a lack of understanding by family, friends, physicians, and/or co-workers who need or require you to walk. Sufferers are often subject to comments such as "I've never seen a case like this before" "It's just in your head","You just need to walk more" and my all-time favorite: "If we cut your feet off, it wouldn't hurt anymore and you could walk on the nubs. Here, I've got a knife." Heel pain seems much more likely to be the target of these attitudes than other ailments. Possible reasons for the unusually unkind attitudes toward sufferers with chronic heel pain include (1) the feet get less respect, (2) the invisible nature of the injury, (3) the seemingly never-ending recovery period, (4) not having a specific event to single-out as the cause, and (5) staying off the feet being associated with laziness. Visitors to this site are often grateful to be able to interact with others who have experienced these psychological/social issues. The condition makes many people feel like they are alone. It can be like a terrorist: it's not just the pain, but the looming threat of more pain, affecting every contemplation (not just the final decision) of going anywhere and doing anything. Zoloft and Prozac are two of the most successful anti-depressants. Less-beneficial over-the-counter pills are 5-HTP, St. John's Wort, and Kava. For stress, at least 1,000 mg vitamin C four times a day and a B-100 complex each day are beneficial. Defining the Plantar FasciaIs it a fascia or aponeurosis? The plantar fascia is also called the plantar aponeurosis by twelve percent of the web pages on the Internet that mention either phrase. In some medical dictionaries and in the Oxford English Dictionary, fascia and aponeurosis are synonyms. Taber's Cyclopedic Medical Dictionary says that plantar aponeurosis and plantar fascia are synonyms. Anatomy books refer to it as either the plantar aponeurosis or the plantar fascia, usually without mentioning the other term. As shown by the following definitions, plantar aponeurosis is the more accurate term, but this web site uses the more common term "plantar fascia." Aponeurosis defined: The best definitions I could find for aponeurosis were from common rather than medical dictionaries. Webster's New Riverside University Dictionary (1988): "A sheet-like membrane resembling a flattened tendon that envelops a muscle or connects it to its insertion." Webster's Ninth New Collegiate Dictionary (1984): "any of the thicker and denser of the deep fasciae that cover, invest, and form the terminations and attachments of various muscles and differ from tendons in being broad, flat, and thin." The Oxford English Dictionary: "a white, shining, fibrous membrane, sometimes serving as the sheath of a muscle, sometimes forming the connexion between a muscle and a tendon" and that it originally comes from the Greek (by way of Latin) "to change into a tendon." Taber's: "a flat fibrous sheet of connective tissue that attaches muscle to bone or other tissues; may sometimes serve as a fascia." Encyclopaedia Britannica (15th ed): "a flat sheet or ribbon like piece of tendon-like material that anchors a muscle or connects it with the part that the muscle moves. The aponeurosis is composed of dense fibrous connective tissue containing fibroblasts (collagen-secreting spindle-shaped cells) and bundles of collagen fibres in ordered arrays. Aponeuroses are structurally similar to tendons and ligaments." Deep or superficial fascia? "Fascia" comes from the Latin for "band." Fasciae (the "e" on the end indicates plural) are divided into "superficial" and "deep" fasciae. Webster's defines superficial fascia as "the thin layer of loose fatty connective tissue underlying the skin and binding it to the parts beneath -- called also hypodermis." Taber's states that superficial fascia allows the skin to move freely. Deep fascia is generally agreed to be the sheath that covers muscle and in some circumstances covers other tissue. Deep fascia transforms into tendon as the muscle it surrounds diminishes and only tendon is left as it gets closer to its attachment to bone. The term "plantar fascia" appears to always refer to the deep fasciae in the sole of the foot which encapsulate three specific muscles. The superficial fascia in the sole of the foot is unusually thick. It is unclear if the inflammation indicated by the term "plantar fasciitis" is in the deep fascia, superficial fascia, or both. The deep fascia probably endures much more tension than the superficial fascia. This web site uses the term "plantar fascia" to refer to the deep plantar fascia, which seems to be the convention used by most other authors. Fascia or fasciae? Since there are three muscles encapsulated by the plantar fascia, plantar fasciae appears to be the more accurate term. However, the three plantar fasciae merge at the heel to form one fascia (or aponeurosis). Of all the web pages found through a search engine, 0.3% use "fasciae" instead of "fascia" when discussing the plantar fascia(e). This web site generally uses "fascia." The plantar fascia.The plantar fascia has three bands or sections: the medial (inside edge of the foot), central, and lateral (outside edge of the foot). These sections are based on which muscles they encapsulate. The medial band encapsulates the "abductor hallucis" (abductor=pull out, hallucis=big toe), the central band encapsulates the "flexor brevis digitorum" (flexor=pull in, brevis=short muscle, digitorum=toes), and the lateral band encapsulates the "abductor minimi digiti" (minimi=smallest, digit=toe). The deep fascia of these three muscles merge where they connect to the heel. Because of the short distance between the muscles and the heel bone, the fasciae have not transformed into tendons as they would have in other areas. Some sources state that heel spurs are not in the fascia, but deeper where the abductor hallucis attaches to the heel bone. I'm not aware of anything other than the fascia that attaches this muscle to the heel, so these sources may be in error. The three bands of the fascia at the heel merge to be 2/3" (17.4mm) wide3 from the medial to central area in front of the heel bone. In dissection of 200 cadavers, Barrett found the fascia to be about 1/8" thick (between 2 and 4 mm), with the medial band roughly twice as thick as the central and lateral bands. The plantar fasciae attachments to the fore foot are complex enough to not discuss, except to say that when the toes bend back, the fasciae tighten. The plantar aponeurosis. Gray's Anatomy, 36th edition, 1980 (as opposed to the much older and cheaper paperback version of Gray's Anatomy sold in bookstores), states that the area of the plantar fascia we are concerned with (the sheet-like portion exterior to the muscles on the bottom of the foot) is usually called the plantar aponeurosis. It says some anatomists define only the central band as the plantar aponeurosis, but that the medial and lateral bands' of the fascia are also aponeurotic (thicker and denser) as they get closer to the heel bone. This shows that "plantar fascia" and "plantar fasciitis" are incorrect and that the correct term for plantar fasciitis is actually "plantar aponeurositis," which, to my knowledge, is never used. How the term "heel spur" comes into play is complex as discussed in a previous section, but the simplified story is that this phrase is the most commonly used because it is the easiest to pronounce and because a spur can often be seen on an x-ray. Calculating Tension in the FasciaThis section is the most difficult to understand, but it explains very precisely why heel lifts, soft floors, arch support, stretching, losing weight, and flexible shoes are good treatments.If the foot is modeled as a simple truss, during normal slow walking the maximum tension in the fascia occurs just as the heel leaves the ground and is equal to Tmax = W*Q/H where W is body weight, H is the height of the ankle pivot point above the ground, and Q is the distance on the ground from directly below the ankle pivot point to the average point of force under the ball.  W comes from the fact that all the body weight is on one foot right before the heel comes off the ground. The Q/H ratio is a measure of how hard it is for the truss (i.e., foot) to "tip over" just before the heel comes off the ground ("heel-off"). After heel-off, the windlass mechanism (see running section) keeps Q about the same distance. The pushing of the body after heel-off keeps T as high as or higher than Tmax depending on how fast the person is walking and how long the strides are. Stiff shoes effectively increase Q, which increases Tmax. Pronation decreases H and increases Q, both of which increase Tmax, which can be prevented by arch support. In general, arch support will help keep H high and Q low. Heel lifts increase H which lowers Tmax, and losing weight (W) lowers Tmax. Lack of flexibility in the gastroc calf muscle prevents the ankle from being able to pivot correctly which is what allows the body's center of gravity to easily move forward and cause tip over. Heel lifts help alleviate this by giving an extra edge to the limited flexibility by tipping the truss forward a few degrees (increasing H). Without the ankle pivoting due to a tight gastroc, tension in the gastroc transers through the calcaneous to the fascia. The harm is greater on hard surfaces in hard shoes because soft surfaces similate a heel lift as weight on the forefoot lowers the forefoot relative to the heel which raises due to the soft surface springing up to regain its shape. Said another way, soft surfaces prevent a sudden jerk in tension as the heel comes off the ground if there is lack of flexibility in the gastroc. Intrinsic foot muscles are believed to relieve some tension in the fascia. Strong foot musculature may promote foot functioning that indirectly protects the fascia. Ligament tissue superior to the fascia may also bear some of the tension. The tension in the fascia increases from zero as the torso passes over the heel up to Tmax when the torso passes over the toes. The body's center of gravity passing over the point of ground contact with the toes is by definition tip over. The higher a person's center of gravity and shorter their feet, the easier it is for that person to tip over their feet, so that more weight in the hip and thighs would be more dangerous than extra weight around the belly. This may explain why 2/3 of our visitors are women and why overweight women are 6 times more likely than overweight men to visit heelspurs.com. The tension decreases back to zero as the torso (center of gravity) passes over the open space between the feet and then crosses over to the heel of the other foot and the cycle begins again for the next step. During the time in the chart where tension is a max, the distance between the heel and ball is 2.5% greater than when there is no (or minimal) tension. The H distance did not appear to change. This is shown in the 3 images below that were taken from a x-ray video of a foot in action. I drew the chart below based on the distance between the heel bone and ball of the foot as observed frame-by-frame in the video. The distance increases very slowly at first, but increases suddenly just before heel off, apparently as a result of the achilles tightening and an increase in tension in the fascia. The distance should be closely proportional to the fascia tension up until the point where the fascia reaches its maximum length. Thereafter, tension may increase without the distance between the heel and the ball increasing. However, if tension does reach that point, it may be a sign of inflexible calf muscles and a primary cause of plantar fasciitis. I've given an equation for Tmax, but it can be modified slightly to give a theoretical equation for the tension in the fascia from just after the time the heel touches the ground until when the heel leaves the ground: T=W*x/L*Q/H where x is the distance from the center of the heel to where the center of gravity falls through the foot (somewhere between the heel and forefoot) and L is the distance from the heel to the center point of contact in the forefoot. If Q/H were constant and the calf muscles were perfectly flexible, then this equation would give a straight, increasing line from 0 to Tmax, corresponding to the first half of the curve above which differs by showing a sudden bump. When standing, the center of gravity should fall halfway between the heel and forefoot (x/L is about 0.5), so that T=W*Q/H*0.5 which means T in standing is about 50% of Tmax, so that it's safer for those with heel pain to stand than walk. To oversimplify, it may also mean you should be able to stand twice as long as you can walk. Diabetes, Cancer, and Heart DiseaseThis is not about heel pain, but i see so many people suffering and dying from not knowing the following that i wanted to include it. None of the following should interfere with doctor-prescribed medications. They come in pill form, but they are not drugs: they are components of food. For better absorption and consistent blood levels, the doses should be spread out over each day. For diabetes 5,000 mg or more vitamin C, 800 mcg chromium, 1,600 IU vitamin E, Vanadyl Sulfate (possibly toxic?) and 500 mg magnesium. The need for insulin and pills can decrease dramatically -- blood sugar needs to be monitored. For cancer, 10,000 mg or more vitamin C spread out over each day (see note below), along with high doses of vitamins A, E, selenium, other antioxidants, and the B vitamins. For heart disease there are reports that 5,000 mg of lysine and 5,000 mg or more of vitamin C spread out over each day will reverse angina in two to four weeks. Lysine is an amino acid and is perfectly safe at this dose. 800 IU Vitamin E and 200 mg Co-Enzyme Q10 are also very important for heart ailments. 2 or 3 grams of lysine per day and 4 or so g/d of vitamin C is theoretically supposed to prevent dangers from high cholesterol because the lysine binds to cholesterol, but if you don't like seeing high cholesterol, 3,000 mg inositol hexaniacinate and/or 1,000 mg pantethine (but not pantothenic acid) spread out over each day raise HDL (good kind) and lower LDL (bad kind) by large percentages. Inositol hexaniacinate (in the plain niacin form that causes red flushing and tingling) raised HDL and lowered Lp(a) much better than a popularly-prescribed pill. Other forms of time-release niacin cause liver damage. Niacin has been shown to increase life span by the Coronary Drug Project. Inositol hexaniacinate is better than niacin. Diabetics can take pantethine instead because too much inositol hexaniacinate or niacin has been said to alter blood sugar levels, even though a recent JAMA study (JAMA. 2000;284:1263-1270) stated this was not an issue. A can of salmon each week may greatly lower triglycerides. I would never take a doctor prescribed cholesterol-lowering drug because as of January 2004, everything i have heard so far about them over the years tends to make me think they are still highly dangerous and deadly. See also my nutritional supplement rant cure.html. Note: According to three studies, vitamin C increases survival time of cancer patients by a factor of 4. A Mayo Clinic study published in 1979 showed no effect when taken after chemo. The same group published another study in 1985 showing there was no effect even without chemo, but the NEJM, the National Cancer Institute, and the Mayo Clinic failed to mention that none of the patients died while taking vitamin C (Pauling, 1986 "How to Live Longer and Feel Better" p234). My references to this off-topic paragraph would be 10 times longer than the paragraph itself, so I've excluded them. For the most part it comes from Linus Pauling and Michael Murray books which are extremely well-referenced. Comments About DietIn general, I attempt to maintain a low-calorie, low sugar, very low fat, low milk, low wheat, high fiber diet, high fruit, high vegetable, and high legume diet. Lots of supplements too (10 g vit C, 2,000% B-complex, 1,000 IU vit D, 800 vit E, 200 mcg selenium, etc). Low calorie because that's the best way to increase the number of healthy years. Low sugar to prevent heart disease and to prevent wasted calories since I'm on a low calorie diet and I need the nutrition from real food. Low fat because fat causes cancer more than anything else. Also 30 minutes aerobic activity every other day for all of the above health reasons. Sugar, Fat, and the Paleolithic Diet: On a per-gram basis, fat has twice as many calories as sugar, but sugar raises blood sugar quickly which produces a "high". The body turns high blood sugar into body fat. Hunger returns more quickly after a sugar-loaded meal. Sugar (sucrose) has a higher correlation with heart disease than fat in Yudkin's 1971 cross-cultural studies.24, 25 I reviewed the sugar consumption in various countries using the Food and Agricultural Organization's Food Balance Sheets and compared it to the World Health Organization's information on causes of death (both are in databases available online) and found the refined sugar and heart disease correlation to still be true today. Replacing sucrose and fructose in the diet with glucose was shown in 1970 to dramatically reduce cholesterol by 24% in 18 subjects in two weeks.26 50% of sucrose converts to fructose which converts to acetate which partially converts to cholesterol. It has been known at least since 1960 that some cultures consume high amounts of fat but do not get heart disease until they move to countries that regularly consume sugar. Eskimos eating a traditional very high-fat diet do not get heart disease.15 Linus Pauling's excellent 1986 book How to Live Longer and Feel Better emphasizes we should get as much vitamin C as our Paleolithic ancestors and other mammals (2,300 to 10,000 mg/day) and reduce our sugar intake to the levels our ancestors maintained (60 grams a day). He dismisses the popular wisdom that fat in the diet increases heart disease and doesn't mention that it increases the rate of cancer (at least in industrialized countries). Pauling and many others promote a hunter-gatherer, Stone Age, Paleolithic diet of raw(?) meat, fruits, and vegetables that contains more protein, fiber, potassium, calcium, vitamins, minerals, and omega-3 oils and much less fat, sodium, grains, and milk. In addition to the studies showing very little heart disease in non-industrialized cultures with high-fat diets, Dr. Newbold has shown how to dramatically reduce weight and cholesterol (by 28%) and raise HDL on a high animal fat diet that otherwise similates the Paleolithic diet.28, 29, 30 Wild game contains 4% fat rather than the 25% or 30% in domesticated animals,15 but Dr. Newbold doesn't acknowledge this aspect (that true Paleolithic diets did not contain as much animal fat as he is claiming is OK). He emphasizes most methods of meat preparation make the meat and fats harmful. Since agriculture started taking root only 10,000 years ago and spread slowly over thousands of year (and still hasn't reached some cultures), most of us have not yet evolved to tolerate grains, sugar, milk products, and the various ways we now process and store meat and fats. The archaeological record shows a dramatic decline in human health with the spread of agriculture.31 The high incidence of people in the world who are lactose-intolerant in adulthood is an example of genes that have not caught up with the new diet that contains milk. The great improvement in health people may notice when taking larger amounts of vitamin C may be because we evolved on a Paleolithic diet that contained 2300 mg/day15 rather than an RDA of 90 mg/day. The need for calcium supplements (even doctors are recommending them) can also be explained by Paleolithic diet theories. But extreme physical activity was also a part of the hunter-gatherer lifestyle. A well-referenced very low fat diet is detailed in Raymond Kurzweil's 1993 The 10% Solution for a Healthy Life which recommends only 10% of our calories should come from fat rather than the current guideline of 30%. He emphasizes consuming only 20 to 30 grams of fat per day to nearly eliminate obesity, cancer, stroke, and heart disease. He says it's easy to do (he includes recipes). He cites several studies that show a very low fat diet reverses arteriosclerosis. I would be careful to get enough essential omega-3 oils from flax seed or cold-water fish such as salmon and albacore. He was not aware of the sugar-cholesterol connection until I emailed him (although his book discourages sugar) and his book did not mention Eskimo and African tribes that have traditional diets high in fat and yet do not often get these diseases.
Part 1heelspurs.com This is the 7/14/2002 version. Copyright © 2004 by heelspurs.com LLC. scott@heelspurs.com |